Pre-eclampsia is a serious condition of pregnancy characterised by high blood pressure, protein in the urine and swelling of the hands, feet and face. Most women with pre-eclampsia don’t have obvious symptoms, so regular antenatal check-ups are vital. The only cure is delivery of the baby.” – Better Health Channel
Pre-eclampsia is a serious condition and the most common medical complication of pregnancy. Many premature babies are born to mothers who have pre-eclampsia during the course of their pregnancy.
The condition is the reason behind one in five labour inductions and one in six caesareans.
Determining who will and won’t develop pre-eclampsia is, unfortunately, not a simple task. There is no way of screening for symptoms, but genetic factors and the condition of the placenta do seem to play significant roles in diagnosis. Pre-eclampsia also tends to be more common in first-time pregnancies.
There are some factors that make women more susceptible to pre-eclampsia, alongside first-time pregnancies. These are:
-
Women with pre-existing high blood pressure;
-
Women with a type/ types of vascular disease;
-
Women with a family history pre-eclampsia;
-
Women with diabetes;
-
Women expecting multiple babies;
-
Women over 40 years old;
-
Women who were very obese at the start of their pregnancy (BMI of 35 or more);
-
Women with pre-existing kidney problems;
-
Women with lupus (diseases or conditions marked by inflammation of the skin);
-
Women who have a family history of pre-eclampsia (for example their mother or sister);
-
Women who have experienced pre-eclampsia in previous pregnancies; and,
-
Women who have a new partner who has experienced pre-eclampsia in previous pregnancies (with a previous partner).
Once the baby and placenta are delivered, the mother’s blood pressure and symptoms usually return to normal. This is because the only way of curing the condition is to deliver the baby as soon as possible.
When does pre-eclampsia develop?
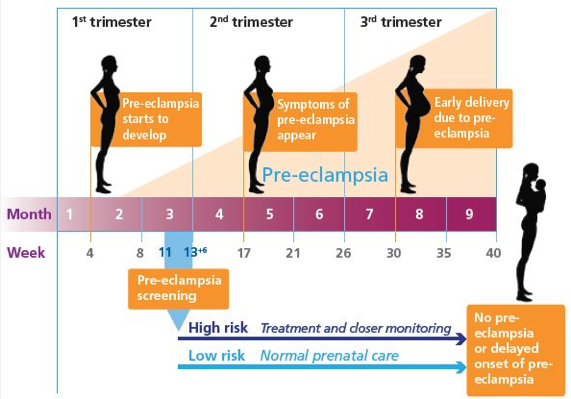
Pre-eclampsia can develop at any stage during the second half of pregnancy. It develops during the later stages of pregnancy in most cases.
A timeline of how pre-eclampsia can develop. Image source: http://www.perkinelmer.com/pages/060/preeclampsia-prevention.xhtml
Although generally there are no definitive signs or ways to predict pre-eclampsia, there are some symptoms mothers should be aware of. When the following symptoms are present during the second half of pregnancy or in the first few weeks after birth, you should visit your doctor:
-
Sudden swelling of the face, hands or feet;
-
Intense headaches accompanied by blurred vision or spots before the eyes;
-
Sever pain in the top of your abdomen; and,
-
Vomiting
What can pre-eclampsia cause?
Pre-eclampsia can cause high blood pressure and protein in the urine. This condition can ultimately have a wide range of effects, which involve most body organs. At its worst, there can be complications to the kidneys, liver, brain and blood.
Blood pressure is measured and compared with your blood pressure taken at the beginning of the pregnancy and subsequent visits. If your blood pressure has increased between visits, your doctor might opt for further tests.
How is blood pressure measured?
Blood pressure is written as a fraction, one number over another – for example 120/80.
The top number indicates your systolic blood pressure, which is the maximum pressure of blood within the blood vessels (veins, arteries etc.). The maximum burst of pressure happens every time your heart beats, because this is when the blood is forced back into circulation by the heart’s contraction.
The bottom number indicates your diastolic blood pressure, which is the pressure measured in between heartbeats.
Keep in mind that there is no ‘normal’ blood pressure – it is different for everyone. What’s important is that the difference, is different to your own general blood pressure rate. The common resting blood pressure reading is 120/80.
There are many factors that affect blood pressure, including: age, gender, activity levels, stress, exercise, sleep and, of course, pregnancy.
Blood pressure is only classified as high when you are resting – it is never measured during an active state. When measuring for high blood pressure the same recording has to be taken multiple times at resting point so as to rule out that it is not an anomaly. Keep in mind that during pregnancy your resting blood pressure is slightly lower than someone who is not pregnant. Once you breach the 140/90 mark when resting, then you are definitely within the high blood pressure range.
During pregnancy the hormones released result in a lower overall blood pressure, because the vessels are relaxed. In pre-eclampsia this is not the case.
In standard pregnancies, mothers can have blood pressure readings as low as 90/60. This does change throughout the different stages of the pregnancy – between early, middle and late pregnancy the blood pressure reading will normally vary.
Generally the pattern is that both systolic and diastolic numbers continue to fall all the way through to 24 weeks. They may rise slightly near delivery time, but even during labour there is usually no increase in blood pressure.
Following these common trends and comparing them, doctors can identify an anomaly in blood pressure and advise more tests if they think your blood pressure is a concern.
These three little early birds are enjoying their time in their onesies.
Will pre-eclampsia affect my baby?
Pre-eclampsia affects the blood supply from the mother to the placenta and does limit the baby’s supply of nutrients and oxygen. This can lead to reduced growth (also known as intrauterine growth restriction) and oxygen deprivation.
With close monitoring, doctors can make sure that intrauterine problems do not develop into worse conditions.
Myths
A common misconception is that pre-eclampsia is caused by stress – whether it be emotional, physical or mental. Some people even think that the condition can be brought about by working too hard or not getting enough sleep – these are common myths.
Pre-eclampsia can range from mild to severe and can affect all different systems and functions of the body. Remembering that it cannot be cured without delivery of the baby, this condition can be managed to an extent. Pre-eclampsia reduces the flow of blood to the placenta, and can be quite dangerous to unborn babies – this is why early birth is usually the next point of action.
A reduced flow of blood impacts on a pregnancy because it restricts a baby’s growth when not enough oxygen or nutrients get through.
If left undetected, pre-eclampsia can lead to eclampsia. Eclampsia is a more serious form of the condition, where the mother’s blood pressure is raised dangerously high. Eclampsia by definition means seizures or convulsions. These can lead to coma and can be fatal.
As mentioned at the beginning of this post, pre-eclampsia affects five to 10 per cent of all pregnancies in Australia. Think of that as about five to 10 women out of 100. In comparison, eclampsia affects only one in 2000 pregnant women – and is therefore much rarer. Out of all cases of eclampsia, half of them occur after the baby is born. In these cases the baby is not so much at risk, compared with the mother.
There is no real way of preventing pre-eclampsia. The best way to stay on top of things is to frequently attend your antenatal appointments. The main reasons for doctors conducting urine and blood pressure tests during these appointments, is to detect any early signs of pre-eclampsia.
Preventative measures
There is evidence that in some cases, regular low-dose aspirin and calcium supplements taken before and in early pregnancy can help prevent pre-eclampsia.
There are also some prescribed drugs that can help with high blood pressure, and magnesium sulphate injections are also proven to help.
The most common prescription drugs in Australia are:
-
Clonidine/Methydopa;
-
NifedipinE;
-
Hydraiazine;
-
Diazoxide;
-
Oxprenolol; and,
-
Labetolol.
All of the above aim to reduce blood pressure, but work in different ways. Usually a combination of two at lower doses is more effective than one at a higher dose. This is a good way of minimising side effects from the medication. All work differently for different people and some can be more effective than others.
What happens after I am diagnosed?
If your blood pressure is only moderately high, bed rest is the best option. While resting, lying on your left-hand side is usually proven helpful because it improves the flow of blood to the placenta. Aside from this, sitting propped up also helps lower blood pressure.
If you have been told you have slightly raised blood pressure (not diagnosed high blood pressure), you will most likely be asked to visit your doctor two or three times a week to have your blood pressure and general health checked.
If your blood pressure becomes any higher, the next step is to go to hospital so doctors and nurses can monitor yours and the baby’s condition. The ultimate aim by moving you into monitored care is to prolong the pregnancy, because the more time babies have in the womb the better. However if doctors deem it necessary, early birth is usually the solution to pre-eclampsia and eclampsia. This is either done by caesarian section or induced labour.
This little bub still requires oxygen, but is just happy snuggling up next to dad.
Are there long-term effects?
The majority of pre-eclampsia cases result in no adverse long-term effects following the baby’s delivery. Occasionally there can be some organ damage that remains for the mother after the disease is essentially cured following birth.
For the babies there are usually no long-term health problems, unless they have suffered severe nutrient starvation or oxygen deprivation in the womb or have been troubled by complications of prematurity.
Aside from leading to eclampsia, pre-eclampsia can be involved with complications such as HELLP syndrome.
HELLP syndrome
HELLP syndrome is a liver and blood clotting disorder. It can result as a complication of pre-eclampsia, or it can develop before pre-eclampsia has even been diagnosed.
HELLP stands for:
H aemolysis – breaking down of red blood cells,
E levated,
L iver enzymes – indicating liver damage,
L ow,
P latelet count – leading to a bleeding tendency.
Haemolysis can lead to anemia, which is a condition where the blood cannot carry enough oxygen to supply the whole body.
When you have elevated liver enzymes, it means your liver is not working properly. As a result, your liver cells are inflamed and can leak high amounts of chemicals and enzymes into your blood.
Having a low platelet count puts you at risk of excess bleeding, because platelets are responsible for helping your blood clot.
The symptoms of HELLP Syndrome include headaches, nausea, heartburn and pain in the upper area of your stomach. In severe cases complications include stroke and failure of the kidneys. Despite these facts, hospital monitoring has been proven effective in managing this condition.
The pain and discomfort from this syndrome is not easily remedied – for example the heartburn caused by HELLP syndrome can’t be cured or aided by simple antacids.
Some women also experience similar symptoms to pre-eclampsia, including swelling of the hands, feet and face. On top of this other symptoms include: excessive weight gain, blurry vision, shoulder pain, pain when taking deep breaths, nose bleeds and in serious cases, seizures.
How is HELLP syndrome diagnosed?
Diagnosing this disorder usually occurs through blood testing – where liver enzymes, red blood cells, and platelets are counted and examined.
Treatment
Similar to pre-eclampsia, the only treatment for HELLP syndrome is delivery of the baby. No matter what stage of the pregnancy, early delivery is essential. Remembering that one of the symptoms of the syndrome is a low platelet count, extreme caution has to be taken when considering any surgery – especially C-section deliveries. Sometimes a platelet transfusion may even be necessary, as platelet deficiency can result in large blood loss through surgery, because blood doesn’t clot properly.
Depending on the severity of the condition, there are cases where doctors may choose not to deliver the baby straight away. In these instances there are a few things that may be recommended:
-
Bed rest (at home or in hospital);
-
Blood transfusions to treat anemia and low platelets;
-
Magnesium sulfate to prevent seizures;
-
Antihypertensive medication to control blood pressure; and,
-
Corticosteroid medication to help the baby’s lungs mature in case an early delivery is required.
When can it occur?
HELLP syndrome usually occurs in the last trimester of pregnancy, before the 37th week. It can also occur after the baby is born in the first week after delivery.
Now you know the signs to look out for regarding pre-eclampsia and HELLP syndrome. If you feel concerned regarding your pregnancy at all, do go and see your doctor.
These three little early birds are enjoying their time in their onesies.
References:
PEARLS Heart Research Institute. Visit www.preeclampsia.org.au.
Australian Action on Pre Eclampsia. Visit www.aapec.org.au.
Tommy’s. Visit www.tommys.org.
Better Health Channel. Visit www.betterhealth.vic.gov.au.
The Royal Women’s Hospital. Visit www.thewomens.org.au.